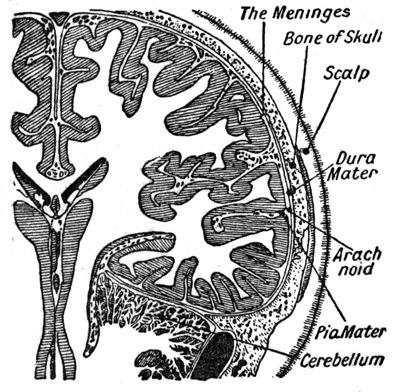
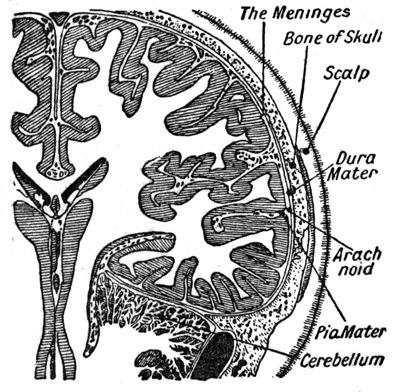
Meningitis, sometimes called spinal meningitis, is an infection of the meninges, the coverings of the brain and spinal cord. In particular, the infection is generally centered in the cerebrospinal fluid, the fluid surrounding the brain and spinal cord in the subarachnoid space. Therefore this is not an infection of the brain or spinal cord itself. However, it can have a profound effect on the adjacent nervous system. Transmission of the causative bacteria or viruses can generally occur by direct contact with an infected individual or from spread through the bloodstream from another source. More information about symptoms can be found on the MeningitisSymptoms page. More information about treatment can be found on the Treatment page. The optimal management of each patient can vary considerably depending on the type of infection that is present. Therefore, each patient should consult their own treating physicians regarding the recommended course of treatment. While bacterial meningitis is a severe, life-threatening disease, viral meningitis tends to be more mild and is rarely life-threatening. Most patients recover fully after the virus runs its course. The treatment and prognosis of each patient may vary. Please consult your own treating physician regarding the appropriate management in your case Bacterial meningitis is one of the most severe forms of meningitis and is life-threatening if not treated promptly. It is a true medical emergency. Another common cause of meningitis are viruses. To learn more about viral causes, see the Viral Meningitis page. There are probably several reasons that a brain aneurysm can develop but one of the most commonly cited is high blood pressure. Because the wall of the aneurysm is under pressure, it gets thinned out and can be prone to bleeding. While aneurysms can occur any time in life, the majority of them present in late adulthood. Aneurysms of the brain blood vessels are not uncommon, but many people have then and never know it. For some percentage of people with aneurysm, the aneurysm leads to symptoms or ruptures, bringing it to medical attention. When a brain aneurysm ruptures, the most common effect is something called subarachnoid hemorrhage. The subarachnoid space is a fluid-filled space between the arachnoid membrane, one of the coverings of the brain and spinal cord, and the surface of the brain. Because the blood vessels to the brain run through this area, when an aneurysm ruptures, it typically bleeds into this space, spreading out through the cerebrospinal fluid. The headache can be accompanied by other signs of irritation of the nervous system including stiff neck, pain with bright lights, nausea and vomiting. In severe cases, hemorrhage can lead to a depressed level of consciousness, coma or even sudden death. In fact, a significant percentage of victims of a ruptured brain aneurysm died before getting to the hospital. Occasionally, the aneurysm itself can cause symptoms if it pushes on nervous system structures as it grows. This can lead to various abnormalities depending on the location of the aneurysm. In some patients, a brain aneurysm may be diagnosed prior to rupture. This can happen incidentally. For example, if a patient is having headaches or some other unrelated symptom that prompts a CT scan or MRI scan, the aneurysm may be found on that scan. Some aneurysms that are causing neurological symptoms may also prompt one of these neurological tests which reveal the aneurysm. In either case, the definitive diagnosis of a cerebral aneurysm is usually confirmed on some form of cerebral angiogram. A traditional angiogram involves placing a catheter through an artery in the leg up into an artery that supplies the brain. Contrast dye which can be seen on x-ray is then injected to visualize the blood vessels in the head while x-rays are taken. This allows a very detailed analysis of the anatomy of the brain blood vessels and can reveal an aneurysm as well as other forms of cerebrovascular disease such as an arteriovenous malformation. Some hospitals now use a less invasive form of angiography called a CT-Angiogram. In this study, contrast dye is simply injected into a normal vein IV and a CT scan of the head is performed at the same time. This allows visualization of the blood vessels as well and a three dimensional reconstruction can be viewed on a computer to see the detailed anatomy of the brain's blood supply. That being said, there are generally a few options for treatment of an aneurysm. Aymptomatic, unruptured aneurysms are sometimes just watched. Alternatively, they may be treated as described below. Again, this decision is made by the patient while discussing the appropriate options with their physician. In the case that treatment is planned for a ruptured or un-ruptured aneurysm, there are generally two primary forms of treatment for most basic aneurysms, although some special cases may require other types of treatment. For ruptured aneurysms, treatment is generally recommended if the patient's condition is stable to help prevent re-bleeding, which can occur in the acute period following a bleed. The traditional way to treat an aneurysm is by a surgery called clipping. The aneurysm is exposed through an opening in the head. The base of the aneurysm, where it bulges off of the normal blood vessel, called the aneurysm neck, is clipped with a special metallic device called an aneurysm clip. This closes the opening into the aneurysms so that blood cannot get into the sac. This clip is left in place permanently. If properly place, it prevents any further enlargement or rupture of the aneurysm. A newer treatment, called coiling, can be done without an open surgical procedure. It is an endovascular treatment which means that it is performed completely from within the blood vessel. A catheter is placed into a large artery, usually in the leg, and a small catheter is maneuvered up into the head and into the aneurysm. Tiny metallic coils are then deployed into the aneurysm which slowly fill the aneurysm from the inside. This is aimed at causing occlusion of the aneurysm so that blood cannot enter it. There is much debate about which treatment for cerebral aneurysm is best, surgical clipping or endovascular coiling. Both have some advantages and disadvantages so no generalization can be made about which is best in all cases. The decision for each patient is made individually based on the specifics of each case and a discussion of the patient or patient's family with their treating physicians. In general, hydrocephalic conditions are separated into two categories: Below you will find a list of types of CSF abnormalities with links to more information about each: Learn about the surgical procedures which are commonly used to treat various forms of hydro: If you cannot find a particular type of hydrocephalic disease, use our Site Map and Search function to search this site. If you still cannot find it, it is possible we do not yet have an article for that specific condition. If that is the case, please Contact Us and let us know. We work hard to post new material often so that we can meet the needs of all of our readers.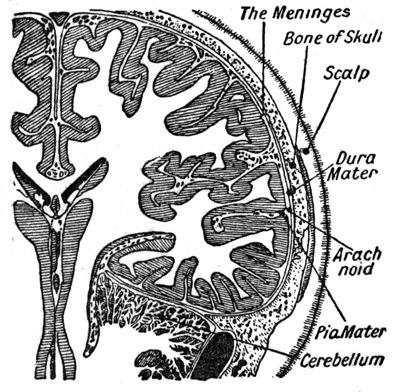
There are several types, generally separated by the causative organism which cases the infection. The most common types are bacterial and viralin origin. Less commonly, infection in this area can be caused by various fungal organisms.What Types of Symptoms Are Typical?
The most common symptoms include headache, neck pain/stiffness, photophobia (avoidance of bright lights), nausea and vomiting and fever. As it progresses, the patient generally has a deterioration of their level of consciousness, particularly with bacterial forms of the disease.How Is The Diagnosis Typically Made?
If a patient presents with signs and symptoms that are typical of this type of CNS infection, a lumbar puncture is generally performed. A lumbar puncture, or spinal tap, is a procedure which introduces a thin needle into the space in the spine where cerebrospinal fluid can be collected. The fluid is sent to a laboratory to be evaluated for several things, including levels of glucose and protein. Additionally, the fluid is examined microscopically to assess for the presence of white blood cells and bacteria. Finally, the fluid is cultured to attempt to isolate and identify the causative organism.What Are Some Common Treatments?
Treatment for general, uncomplicated meningitis depends on the type.Viral causes are generally treated supportively and are self-limited in nature. Bacterial causes must be treated aggressively with intravenous antibiotics. These patients are generally hospitalized and given intravenous antibiotics until the infection has been controlled.Viral Meningitis
What Types of Symptoms Are Typical?
Meningitis symptoms generally include headache, high fever, stiff and/or painful neck, photophobia (avoidance of bright lights), nausea and vomiting and, less commonly with viral disease, deteriorating level of consciousness. However, the symptoms of viral forms of meningitis tend to be much more mild than in bacterial forms of the disease. Fever is generally low grade and nausea and vomiting is less common. Most notably, the level of consciousness is rarely significantly affected by viral infection.How Is The Diagnosis Typically Made?
If a patient presents with the signs and symptoms of meningitis they generally undergo an lumbar puncture (spinal tap) to obtain cerebrospinal fluid for analysis. This can help to distinguish viral from bacterial meningitis. Some of the chemistries tested are different and no bacteria is seen or cultured from the cerebrospinal fluid. This helps confirm the diagnosis of viral meningitis.What Are Some Common Treatments?
Antibiotics are not effective against viruses and therefore are not indicated in the treatment of viral forms of meningitis. In fact, no direct treatment is generally needed because the viral infection is self-limited, meaning it runs its course and then burns out. Generally, viral infection is not life-threatening and hospitalization is not required. Only general supportive care and rest are recommended to most patients. Most recover fully within 2 to 3 weeks without permanent deficits.Bacterial Meningitis
In adults, the most common causative organisms responsible for this disease include Neisseria meningitides and Streptococcus pneumoniaalthough several other bacteria can be implicated, including Haemophilus influenza, tuberculosis, gram negatives, Listeria monocytogenes and others.What Types of Symptoms Are Typical?
Meningitis symptoms generally include headache, high fever, stiff and/or painful neck, photophobia (avoidance of bright lights), nausea and vomiting and deteriorating level of consciousness.How Is The Diagnosis Typically Made?
If a patient presents with the signs and symptoms of meningitis they generally undergo an lumbar puncture (spinal tap) to obtain cerebrospinal fluid for analysis. This can help make the diagnosis of bacterial infection as well as help to guide treatment by isolating the causative organism so that antibiotic therapy can be tailored to the specific case.What Are Some Common Treatments?
Antibiotics directed toward the causative bacteria is the mainstay of treatment along with general supportive measures. The patients are generally hospitalized and antibiotics are given intravenously. The exact type and duration of treatment can vary from patient to patient depending on the severity of disease and the type of causative organismBrain Aneurysm
(Cerebral Aneurysm)What Types of Symptoms Are Typical?
The most common presentation of a brain aneurysm is rupture, causing subarachnoid hemorrhage. The classic presentation of this bleeding is a sudden onset of a severe, excruciating headache. Patients often describe it as the "worst headache of my life" and say it is unlike any other headaches they have had. I comes on quickly and is often described as a severe stabbing or shock-like pain.How Is The Diagnosis Typically Made?
Many brain aneurysms first present themselves when they rupture, presenting with sudden onset of severe headache, neck stiffness, and/or depressed level of consciousness. This presentation usually leads to work-up with a CT scan which can reveal the subarachnoid blood. In some cases where CT is either not available or does not show any obvious blood, a lumbar puncture (spinal tap) is performed to obtain cerebrospinal fluid to analyze it for blood or blood breakdown products. This involves inserting a small needle into the spinal canal through the low back to remove a small amount of cerebrospinal fluid.What Are Some Common Treatments?
Treatment for a brain aneurysm is highly variable, depending on the type and location of the aneurysm, whether it has ruptured or not and details of the patient's condition. Each case should be evaluated by that patient's own physicians to determine the best course of action.All About Hydrocephalus
Wednesday, March 31, 2010
Viral meningitis, also called aseptic meningitis, is a common form of meningitis, infection of the coverings of the brain and spinal cord, caused by various types of viruses.
Bacterial meningitis is a common form of meningitis, infection of the coverings of the brain and spinal cord, caused by various forms of bacteria. The bacteria grow primarily in the subarachnoid space in the cerebrospinal fluid, causing inflammation of the surrounding structures.
A brain aneurysm, or cerebral aneurysm, is an abnormal bulging out of the wall of a blood vessel that brings blood to the brain. Over time, the blood pressure inside the aneurysm can lead to expansion and eventual rupture of the aneurysm.
Hydrocephalus is an abnormality of the normal dynamics of the cerebrospinal fluid (CSF). The CSF is a water-like fluid that surrounds the brain and spinal cord. Normally, it is produced, flows throughout the open spaces in and around the central nervous system (the ventricles and subarachnoid space) and is then re-absorbed. However, some conditions can lead to the accumulation of this fluid or other abnormalities in its flow which can damage the brain and lead to significant symptoms.
Labels: Meningitis
Subscribe to:
Post Comments (Atom)
0 comments:
Post a Comment