| Pneumothorax | |
|---|---|
| Classification and external resources | |
 Chest X-ray of Left-sided Tension Pneumothorax | |
| ICD-10 | J93., P25.1, S27.0 |
| ICD-9 | 512, 860 |
| DiseasesDB | 10195 |
| MedlinePlus | 000087 |
| eMedicine | emerg/469 |
| MeSH | D011030 |
Pneumothorax is a medical condition and potential emergency wherein air or gas is present in the pleural cavity (chest). It may occur spontaneously both in people with chronic lung conditions and those with no other health problems, but many pneumothoraces occur after physical trauma to the chest, blast injury, or as a complication of medical treatment. In the past, creating a pneumothorax was used as a treatment for various lung disorders, such as tuberculosis; this has now been abandoned.
The symptoms of a pneumothorax are determined by the size of the air leak and the speed by which it occurs; they may include chest pain and shortness of breath in most cases, and fainting and rarely cardiac arrest in severe cases ("tension pneumothorax"). The diagnosis can be made by physical examination in severe cases but usually requires a chest X-ray in milder forms.
Small pneumothoraces typically resolve by themselves and require no treatment. In larger pneumothoraces or when there are severe symptoms, the air may be aspirated with a syringe, or a one-way chest tube is inserted to allow the air to escape. Occasionally, surgical measures are required, especially if tube drainage is unsuccessful.
Pneumothorax presents mainly as a sudden shortness of breath, dry coughs, cyanosis (turning blue) and pain felt in the chest, back and/or arms. In penetrating chest wounds, the sound of air flowing through the puncture hole may indicate pneumothorax, hence the term "sucking" chest wound. The flopping sound of a punctured lung is also occasionally heard.Subcutaneous emphysema is another symptom.
Signs and symptoms
If untreated, hypoxia may lead to hypercapnia, respiratory acidosis, and loss of consciousness. In a tension pneumothorax, shifting of the mediastinum away from the site of the injury can obstruct the superior and inferior vena cavaresulting in reduced venous return. This in turn decreases cardiac preload and cardiac output.
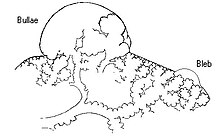
Spontaneous pneumothorax has been reported in young people with a marfanoid habitus. The reason for this association, while unknown, is hypothesized to be the presence of subtle abnormalities in connective tissue, though not necessarily inelastin per se. Most spontaneous pneumothorax result from "blebs", expanded alveoli just under the superficial surface of the lung, that rupture allowing the escape of air into the pleural cavity.
Pneumothorax can also occur as part of medical procedures, such as the insertion of a central venous catheter into thesubclavian vein. Other causes include mechanical ventilation, endotracheal intubation, laparoscopic surgery, emphysemaand less commonly other lung diseases bacterial or viral (pneumonia), metastatic tumors especially sarcomas, lymphangioleiomyomatosis, eosinophilic granuloma, cystic fibrosis, alpha1-antitrypsin deficiency, spontaneous or traumatic esophageal rupture, Pneumocystis carinii pneumonia, lung abscess, and asthma[1].
Cause
It most commonly arises:
- Spontaneously (more commonly in tall slim young males and in Marfan syndrome)
- Following a penetrating chest wound
- Following barotrauma to the lungs[2][3]
It may also be due to:
- Chronic lung pathologies including emphysema, asthma
- Acute infections
- Chronic infections, such as tuberculosis
- Lung damage caused by cystic fibrosis
- Lung Cancer
- Rare diseases that are unique to women such as Catamenial pneumothorax(due to endometriosis in the chest cavity) and lymphangioleiomyomatosis (LAM).
Pneumothoraces are divided into tension and non-tension pneumathoraces. Atension pneumothorax is a medical emergency as air accumulates in the pleural space with each breath. The increase inintrathoracic pressure results in massive shifts of the mediastinum away from the affected lung compressing intrathoracic vessels. A non-tension pneumothorax by contrast is of lesser concern because there is no ongoing accumulation of air and hence no increasing pressure on the organs within the chest.
The accumulation of blood in the thoracic cavity (hemothorax) exacerbates the problem, creating a hemopneumothorax.
Spontaneous pneumothorax
Spontaneous Pneumothorax can be classified as primary spontaneous pneumothorax and secondary spontaneous pneumothorax. In primary spontaneous pneumothorax, it is usually characterized by a rupture of a bleb in the lung while secondary spontaneous pneumothorax mostly occurs due tochronic obstructive pulmonary disease (COPD).
- Primary
A primary spontaneous pneumothorax may occur without either trauma to the chest or any kind of blast injury. This type of pneumothorax is caused when a bleb (an imperfection in the lining of the lung) bursts causing the lung to deflate. The lung is reinflated by the surgical insertion of a chest tube. A minority of patients will suffer a second instance. In this case, thoracic surgeons often recommend thorascopic pleurodesis to improve the contact between the lung and thepleura. If multiple and/or bilateral occurrences continue, surgeons may opt for a far more invasive bullectomy andpleurectomy to permanently adhere the lung to the interior of the rib cage with scar tissue, making collapse of that lung physically impossible. Primary spontaneous pneumothorax is most common in tall, thin men between 17 and 40 years of age, without any history of lung disease. Though less common, it also occurs in women, usually of the same age and body type. The tendency for primary spontaneous pneumothorax sufferers to be tall and thin is not due to weight, diet or lifestyle, but because the genetic predisposition toward those traits often coincides with a genetic predisposition toward high volume lungs with large, burstable blebs. A small portion of primary spontaneous pneumothoraxes occur in persons outside the typical range of age and body type.
- Secondary
In secondary spontaneous pneumothorax, a known lung disease is the cause of the collapse[4]. The most common cause is chronic obstructive pulmonary disease (COPD) with emphysematous bullae. However, there are several other diseases that may also lead to spontaneous pneumothorax:
- Tuberculosis
- Pneumonia
- Asthma
- Cystic fibrosis
- Lung cancer
- Interstitial lung disease
- Marfan syndrome
- Lymphangioleiomyomatosis (LAM)[5]
Differential diagnosis
When presented with this clinical picture, other possible causes include:
- Acute Myocardial Infarction: presents with shortness of breath and chest pain, though MI chest pain is characteristically crushing, central and radiating to the jaw, left arm or stomach. Whilst not a lung condition, patients having an MI often happen to also have lung disease.
- Emphysema: here, delicate functional lung tissue is lost and replaced with air spaces, giving shortness of breath, and decreased air entry and increased resonance on examination. However, it is usually a chronic condition, and signs are diffuse (not localised as in pneumothorax).
Careful history taking and examination and a chest X-ray will allow accurate diagnosis.
Pathophysiology
The lungs are located inside the chest cavity, which is a hollow space. Air is drawn into the lungs by the diaphragm (a powerful abdominal muscle). Thepleural cavity is the region between the chest wall and the lungs. If air enters the pleural cavity, either from the outside (open pneumothorax) or from the lung (closed pneumothorax), the lung collapses and it becomes mechanically impossible for the injured person to breathe, even with an open airway. If a piece of tissue forms a one-way valve that allows air to enter the pleural cavity from the lung but not to escape, overpressure can build up with every breath; this is known as tension pneumothorax. It may lead to severe shortness of breath as well as circulatory collapse, both life-threatening conditions. This condition requires urgent intervention.
Diagnosis
The absence of audible breath sounds through a stethoscope can indicate that the lung is not unfolded in the pleural cavity. This accompanied by hyperresonance (higher pitched sounds than normal) to percussion of the chest wall is suggestive of the diagnosis. The "coin test" may be positive. Two coins when tapped on the affected side, produce a tinkling resonant sound which is audible on auscultation.[6]
If the signs and symptoms are doubtful, an X-ray of the chest can be performed, but in severe hypoxia, or evidence of tension pneumothorax emergency treatment has to be administered first. An x-ray can illustrate the collapse of the lung as extra black space, indicating the presence of air, will be seen in the x-ray around the lung. The lung shrivels up away from the affected side and the mediastinum (trachea and other components) will shift towards the unaffected side.[7]
In a supine chest X-ray the deep sulcus sign is diagnostic[8], which is characterized by a low lateral costophrenic angle on the affected side.[9] In layman's terms, the place where rib and diaphragm meet appears lower on an X-ray with a deep sulcus sign and suggests the diagnosis of pneumothorax.
In Neonates the use of a transilluminator to suspected area will help visualize the air as radiating rings from light source out.
More recently, ultrasound has been shown to be more sensitive than anteroposterior x-ray for detection of pneumothorax. This is important in the initial evaluation of these patients, when the posteroanterior and lateral x-ray studies may not be obtainable due to the patient's clinical condition.[
Management
Chest wound
Penetrating wounds (also known as 'sucking chest wounds') require immediate coverage with an occlusive dressing, field dressing, or pressure bandage made air-tight with petroleum jelly or clean plastic sheeting. The sterile inside of a plastic bandage packaging is good for this purpose; however in an emergency situation any airtight material, even the cellophane of a cigarette pack, can be used. A small opening, known as a flutter valve, may be left open so the air can escape while the lung reinflates. Any patient with a penetrating chest wound must be closely watched at all times and may develop a tension pneumothorax or other immediately life-threatening respiratory emergency at any moment. They cannot be left alone.
Blast injury or tension
If the air in the pleural cavity is due to a tear in the lung tissue (in the case of a blast injury or tension pneumothorax), it needs to be released. A thin needle can be used for this purpose, to relieve the pressure and allow the lung to reinflate.
Pre-hospital care
Many paramedics can perform needle thoracocentesis to relieve intrathoracic pressure. Intubation may be required, even of a conscious patient, if the situation deteriorates. Advanced medical care and immediate evacuation are strongly indicated.
An untreated pneumothorax is an absolute contraindication of evacuation or transportation by flight.
Small pneumothoraces
Small pneumothoraces are often managed conservatively as they will resolve on their own.[11] Repeat observation via chestX-rays and oxygen administered.[12]
Pneumothoraces which are too small to require tube thoracostomy and too large to leave untreated, may be aspirated with a small catheter.
Larger pneumothoraces
Large pneumothoraces may require tube thoracostomy, also known as chest tube placement. If a thorough anesthetizing of the parietal pleura and the intercostal muscles is performed, the only major pain experienced should be either the injury that caused the pneumothorax or the re-expanding of the lung. Proper anesthetizing will come about by the following procedure: the needle should be inserted into the chest cavity and a negative pressure created in the syringe. While air bubbles rise into the syringe, the needle should be slowly pulled out of the cavity until the bubbles cease. The tip of the syringe that contains the anesthetic is now in the intercostal muscles just next to the parietal pleura. A proper and sizable injection should ensue (5 to 10 ml). This will allow the patient to be fairly comfortable despite a hemostat or finger being inserted into the chest cavity. A tube is then inserted through the chest wall into the pleural space and air is extracted using a simple one way valve or vacuum and a water valve device. This allows the lung to re-expand within the chest cavity. The rate of re-expansion will vary widely. It is important not to connect the chest tube to suction right away, as rapid expansion may lead to pulmonary edema. The pneumothorax is followed up with repeated X-rays. If the pneumothorax has resolved and there is no further air leak, the chest tube is removed. If, during the time that the tube is still in the chest, the lung manages to sustain the re-expansion, but once suction is turned off, the lung collapses, a Heimlich valve may be used. This flutter valve allows air and fluid in the pleural cavity to escape the pleura into a drainage bag while not letting any air or fluid back in. This method was developed by the military in order to get soldiers with lung injuries stable and out of the battlefield faster. It is a rarely used medical device in the treatment of patients these days, but may be used in order to allow the patient to leave the hospital.
It is critical that the chest tube be managed in such a way that it does not become kinked or occluded with clot or other fibrinous material. Chest tube clogging can result in build up of air in the pleural space. At the very least, this will lead to a recurrent pneumothorax. In the worse case, the patient can have a tension pneumothorax if the air builds up under pressure and impairs venous return to the heart. This can be fatal. The tubes have a tendency to form clot from blood and other fibrinous material that can occlude them. To keep them open they must be stripped, milked or even replaced if they totally occlude. Smaller tubes are less traumatic, but more prone to clogging, although this can also occur with larger tubes. One sign the chest tube is clogged is subcutaneous emphysema. Another is a loss of respiratory variation in the fluid level at the water seal valve in the drainage canister.
In the situation that the chest tube is not sufficient in healing of the lung (for example, a continued air leak despite chest tube drainage), or if CT scans show the presence of large "bullae" on the surface of the lung, thoracoscopic surgery, orvideo assisted thorascopic surgery (VATS), may be done in order to staple the leak shut and to irritate the pleura to promote adhesions between the lung and pleura (pleurodesis). Two or three small incisions are made in the side of the chest and back, one for a small camera and the other (s) for tools used to seal the lung and abrade or remove the pleura. When finished the wound is covered with a steri-strip and bandaged up.
In case of penetrating wounds, these require attention, but generally only after the airway has been secured and a chest drain inserted. Supportive therapy may include mechanical ventilation.
Surgery
Recurrent pneumothorax may require further corrective and/or preventive measures such as pleurodesis. If the pneumothorax is the result of ruptured bullae, then bullectomy (the removal or stapling of bullae or other faults in the lung) is preferred. Chemical pleurodesis is the injection of a chemical irritant that triggers an inflammatory reaction, leading to adhesion of the visceral pleura, which is in contact with the lung, to the parietal pleura. Substances used for pleurodesis include talc, blood, tetracycline and bleomycin. Mechanical pleurodesis is done by abrading the pleura and does not use chemicals. The surgeon "roughens" up the inside chest wall ("parietal pleura") so the lung attaches to the wall with scar tissue. This can also include a partial "parietal" pleurectomy, which is the removal of the "parietal" pleura; "parietal" pleura is the serous membrane lining the inner surface of the thoracic cage and facing the "visceral" pleura, which lies all over the lung surface. Both operations can be performed using keyhole surgery (VATS) to minimise discomfort to the patient. Sometimes pneumothorax occurs bilaterally in sequence or, more rarely, simultaneously; that is often associated to bilateral apical blebs and obviously requires bilateral treatment.[13][14]
History
Jean Marc Gaspard Itard, a student of René Laennec, first recognised pneumothorax in 1803, and Laennec himself described the full clinical picture in 1819.[15]
Prior to the advent of anti-tuberculous medications, iatrogenic pneumothoraces were intentionally given to tuberculosis patients in an effort to collapse a lobe, or entire lung around a cavitating lesion. This was known as 'resting the lung'.





0 comments:
Post a Comment